Funded Projects
2022 Funded Grants
EWING SARCOMA RESEARCH AT UNIVERSITY OF IOWA STEAD FAMILY CHILDREN’S HOSPITAL
In December of 2022, Sammy's Superheroes Foundation gave $75,000 to the Stead Family Children's Hospital at the University of Iowa.
This grant was designated to the Matt Morrell and Natalie Sanchez Pediatric Cancer Fund and will provide support for the Ewing Sarcoma Research in Dr. Gordan's Lab at the Stead Family Children's Hospital.
Ewing sarcoma is an aggressive bone and soft tissue sarcoma that is treated with highly intensive, cytotoxic chemotherapy in combination with surgery and radiation. The treatment of Ewing sarcoma has changed very little in the past two decades and, unfortunately, even the children who are cured of Ewing sarcoma are left with lifelong side-effects from the therapy. Consequently, there is an urgent and unmet need to identify cancer-specific vulnerabilities that can be targeted to improve the outcomes for children and adolescents with Ewing sarcoma.
LURIE CHILDREN'S FOUNDATION
The board of directors and supporters of Sammy's Superheroes are pleased to award a grant in 2022 for $100,000 in support of Dr. DeCuypere's MD,PhD. research of the BRAF alteration and improving treatment regimens for pediatric brain tumors.
While survival rates for most pediatric cancers have improved significantly during the past four decades, progress in the treatment of aggressive pediatric brain tumors has been limited. There is an urgent need to accelerate discovery and develop better, less toxic therapies to give all children the opportunity for a healthy future. The complex challenges of understanding pediatric brain tumors, some of which are incredibly rare, demonstrate why scientist and physicians at Lurie Children’s are committed to driving clinical and research advances that may one day turn even the most aggressive childhood brain tumors into a curable disease.
2021 Funded Grants
Alex's Lemonade Stand Partnership
In 2021 Sammy's Superheroes Foundation donated $200,000 to Alex's Lemonade Stand Foundation (ALSF).
Sammy's Superheroes Foundation and ALSF share a vision of funding high-impact research to find cures for hard-to-treat childhood cancers. Together we were able to co-fund two cutting-edge research projects.
TARGETING MYCN
$100,000 to Dr. Yael Mossé of the Children's Hospital of Philadelphia
Sammy's Superheroes Foundation is funding Dr. Mossé's Crazy 8 Award, titled Targeting MYCN. Dr. Mossé's goal is to develop targeted drugs for MYCN, a currently "undruggable" driver of pediatric cancer, within the next four years. Dr. Mossé brought together a team of complementary researchers, each with unique experience to attack MYCN with innovative new technologies. Together, they will prove that the drugs they're developing are effective against most lethal pediatric cancers and be ready to launch a clinical trial shortly after the grant is completed in Spring 2025.
'A' AWARD GRANT
$100,000 to Dr. Mariella Filbin of Dana-Farber Cancer Institute in Boston
Sammy's Superheroes Foundation is also funding Dr. Mariella Filbin's 'A' Award Grant, titled Exploiting the Differentiation Potential of Pediatric High-Grade Glioma to Discover Novel Therapeutic Opportunities. Dr. Filbin and her team are using a method called CRISPR-gene editing to ablate specific genes that they've identified as potential antagonists of the developmental programs in both brainstem and hemispheric high-grade gliomas. Dr. Filbin's plan is to identify novel targets for high-grade glioma drug development and lay the foundation for new treatment strategies in this deadly disease.
Ewing sarcoma study at University of Iowa Stead Family Children's Hospital

In December of 2020, we made a $50,000 donation to fund a study being conducted by Dr. David Gordon at the University of Iowa Stead Family Children's Hospital. Dr. Gordon’s lab at U of Iowa specializes in Ewing Sarcoma research. Ewing sarcoma is a cancerous tumor that occurs in or around bone and is the second most common type of bone cancer in children and adolescents. There are currently no known causes or methods of prevention for this type of cancer. Treatments for Ewing sarcoma have not changed in many years, and this study could help improve therapies.
Nebraska Watershed Project
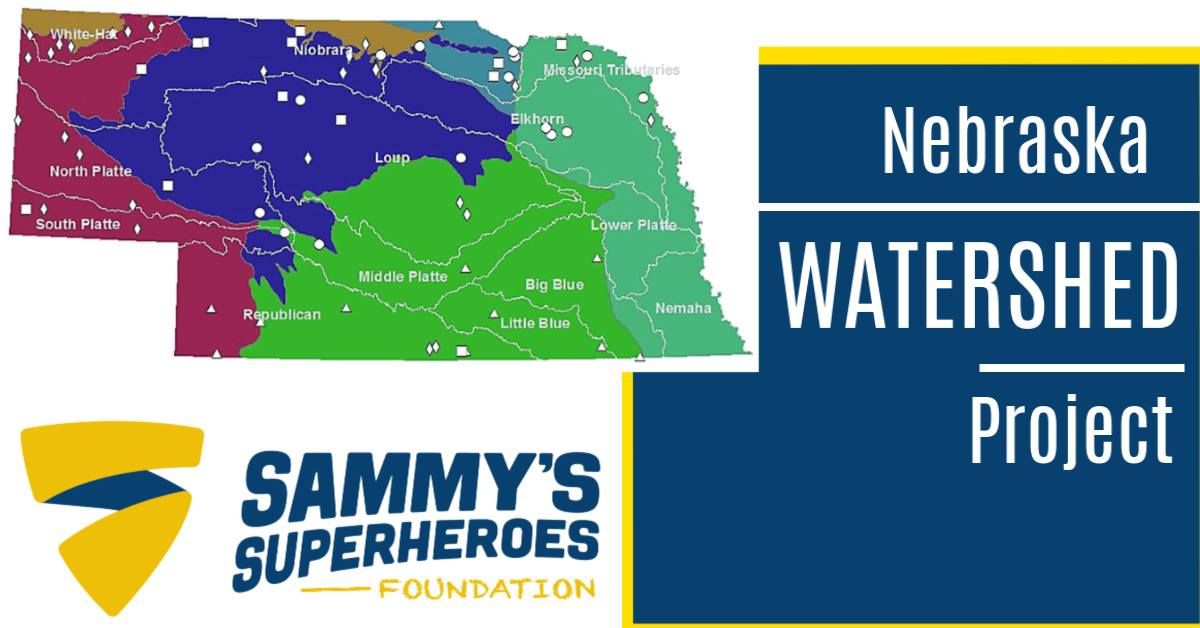
In December of 2019, we completed a $115,000 ($5,000 given in May of 2019) pledge to support a study currently being conducted at University of Nebraska Medical Center, Department of Environmental, Agricultural and Occupational Health College of Public Health. This study focuses on the possible role of contaminants in Nebraska surface and ground waters in the etiology of adverse health conditions, particularly pediatric cancer and birth defects. They will analyze the nitrate data in various ways to relate the levels of pediatric cancers in the approximately 75 watersheds we are using in Nebraska. They are pursuing this investigative approach to try to understand "hotspots" for pediatric cancers and birth defects in Nebraska. Although this study will be an extensive study conducted over many years, Sammy's Superheroes is proud to be a part of making a difference in Nebraska!
Neuroblastoma Project at Dana Farber Institute
In December of 2019, we funded $100,000 to a Neuroblastoma project being conducted at Dana Farber Institute in Boston. Relapsed neuroblastoma refers to the return of neuroblastoma in patients who have already undergone treatment for the disease. Approximately half of children who are treated for high-risk neuroblastoma and achieve an initial remission will have the disease come back. In addition, in approximately 15 percent of children with high-risk neuroblastoma, the tumor does not respond to initial treatment. These children are said to have refractory neuroblastoma. This project is a treatment strategy for residual or refractory neuroblastoma disease, developing a vaccine (GVAX) for patients affected by the disease.
DIPG Project at Lurie Children's Hospital in Chicago
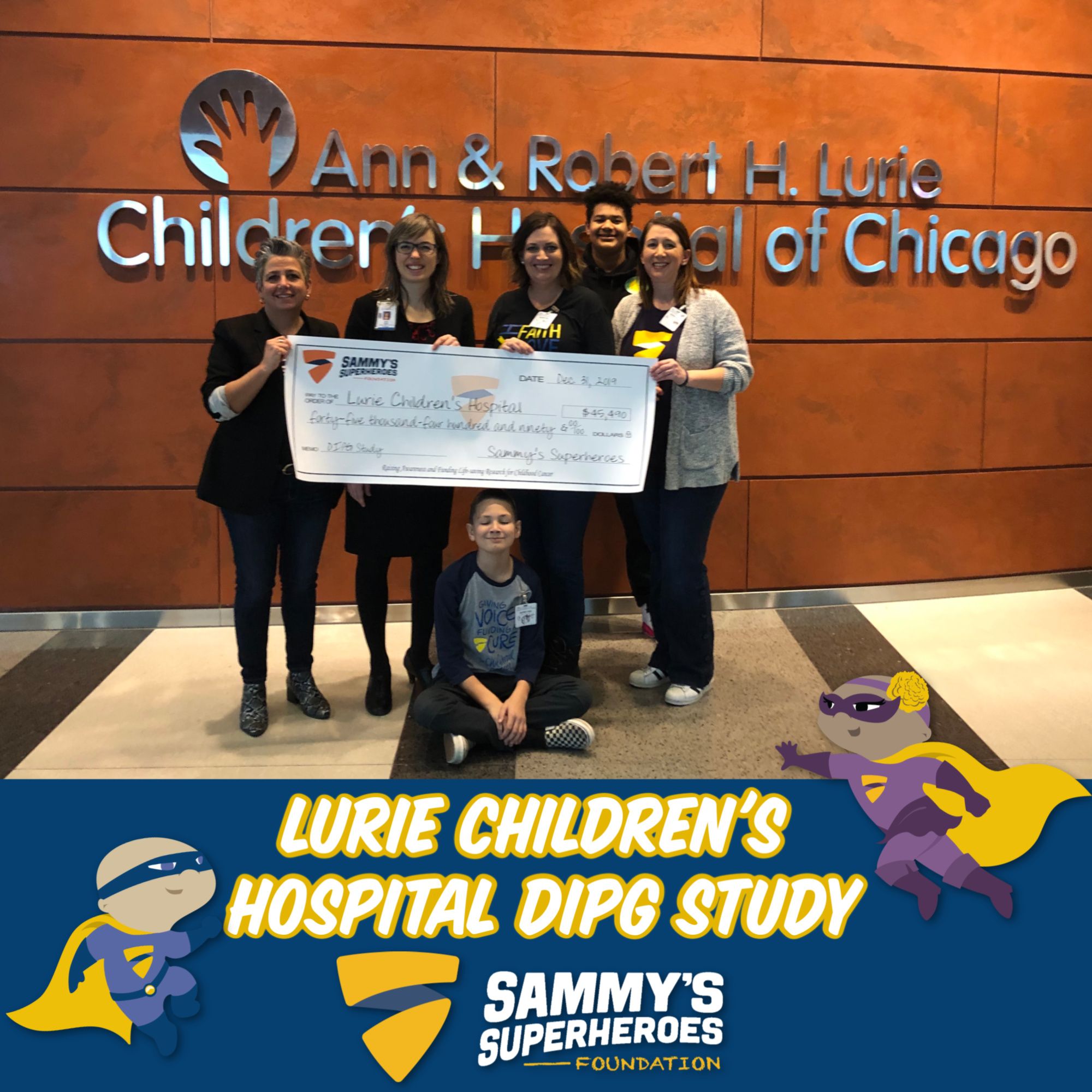
In 2019, we funded $45,490 to a DIPG Project being conducted at Lurie Children's Hospital. DIPG (diffuse intrinsic pontine glioma) is a type of tumor that starts in the brain stem. It is one of the most aggressive and fatal brain tumors of childhood cancer with less than 10% survival one year after diagnosis. At present, there is no cure for this type of tumor. This research will study how Histone 3 (H3) that controls healthy gene expression is mutuated in the majority of high grade gliomas and may be responsible for tumor development using a bromodomain inhibitor the targets the effects of H3 mutation. This is the first treatment strategy of its kind and we are thrilled to be a part of this project.
Pediatric Data Commons Project

In June of 2019, we completed our $400,000 pledge to the University of Chicago's Pediatric Data Commons Project a year early!
Almost 90 percent of kids with the most common types of cancer survive. Yet progress has been limited for many other types of pediatric cancer, such as neuroblastoma, brain tumors, and metastatic sarcoma. Even with modern, intensive treatment approaches, cure rates for high-risk neuroblastoma are less than 50 percent. Much work remains to understand how these tumors resist treatment, and ensure that children with any cancer type experience durable cures.
Comer Children’s Hospital physician-scientist Susan Cohn, MD, is leveraging University of Chicago strengths in big data and basic science research to improve these outcomes. In 2004, she helped form the International Neuroblastoma Risk Group (INRG): a globe-spanning collaborative effort to collect and share data from neuroblastoma research. Today, the INRG database contains information from more than 18,500 patients.
Science rests on the search for patterns. If Newton had only the one apple to go on—instead of a lifetime of watching objects fall—he could never have characterized gravity. For rare conditions like neuroblastoma, researchers have worked from mere handfuls of data points, either because the information wasn’t available or it was available in a form (such as published in journal articles) that couldn’t feasibly be collected and examined together. Dr. Cohn intends to change that with the Pediatric Cancer Data Commons (PCDC). Leveraging the platform built by Robert Grossman, PhD, at the University of Chicago for the Genomic Data Commons—a $38 million National Cancer Institute project to collect, standardize, store, and analyze genomic and clinical information from thousands of cancer patients—the PCDC will link clinical pediatric cancer databases (like the INRG’s) with genomic data and will provide the analytic tools that will help researchers find patterns associating patient genetics and tumor genomics with treatment response and outcome. For example, the PCDC could reveal correlations between certain tumor genetics and patient outcomes, which would lead to better diagnostics: doctors could know, with a biopsy, that patients with specific genetic features would do best with lower doses of chemotherapy.
Check out this article by University of Chicago Medicine and an update on this project: https://www.uchicagomedicine.org/pediatrics-articles/pediatric-cancer-data-commons-aims-to-accelerate-research
Targeting Pediatric AML
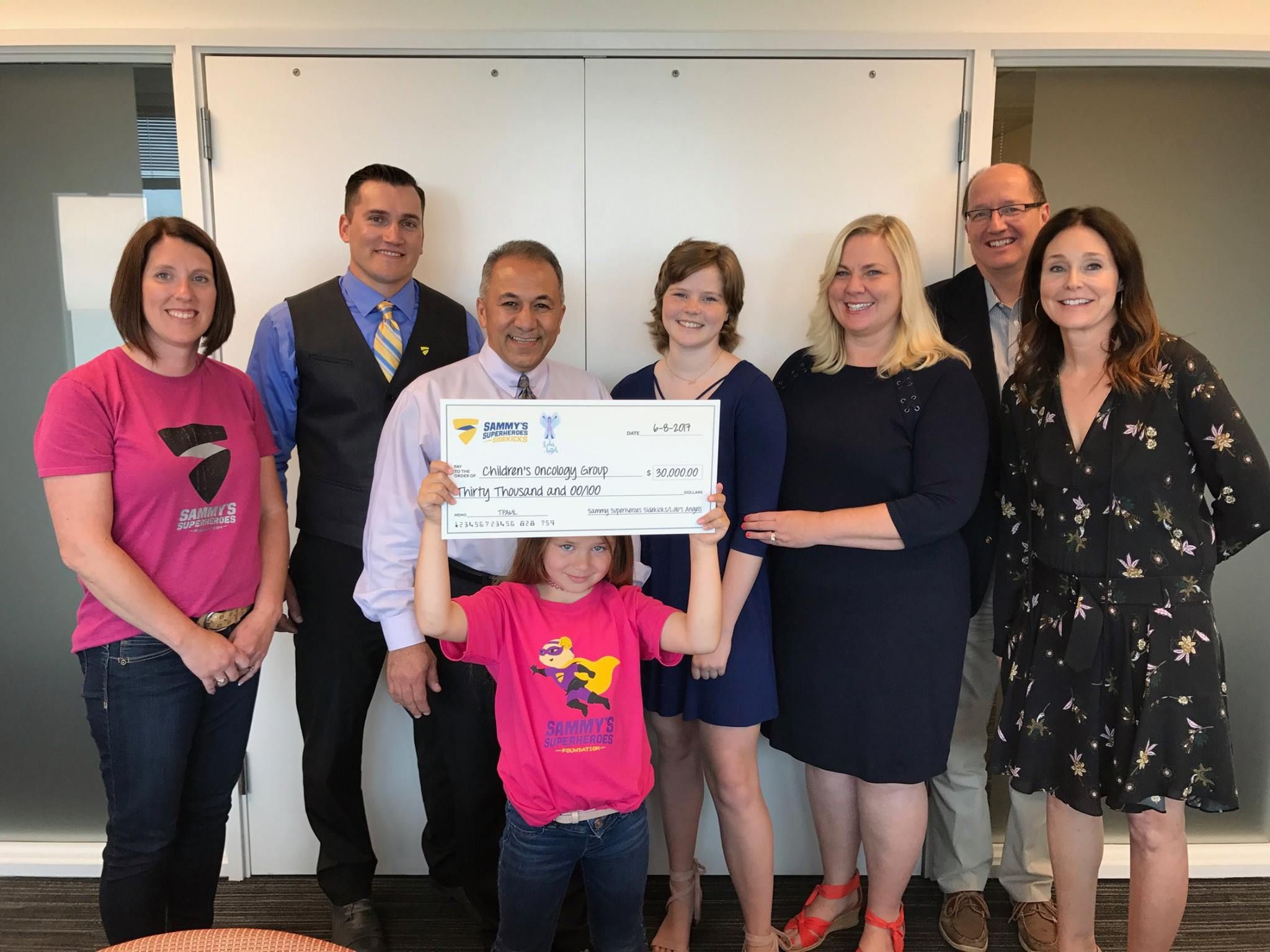
In June of 2017, $30,000 was given to Dr. Soheil Meshinchi in Seattle as our first Sammy's Sidekicks grant! We were excited to work with Lolo's Angels of Omaha, Nebraska, to fund a Target Pediatric AML project.
AML is the deadliest leukemia across all ages. Therapies for AML have not fundamentally changed in decades, so it remains one of the poorest prognoses, most harrowing, and costly pediatric cancers. But targeted agents, like modified T-cells, antibody therapies and small molecule inhibitor drugs, offer the possibility of near-term breakthroughs. However, the applicability and effectiveness of these cutting-edge, precision treatments depend largely on one critical element – identification of GOOD TARGETS. Effective targeting remains a barrier to progress in AML.
TpAML seeks to speed access to promising targeted therapies and begin the shift from the virtual “one- size-fits-all” protocols of today to more personalized, precision treatment regimens tailored to a young AML patient’s specific cancer profile (genetics). This should not only improve outcomes, but reduce both short and long- term treatment-related toxicities. This effort is led by COG Myeloid Disease Committee leaders Dr. Soheil Meshinchi (biology chair) and Dr. Andy Kolb (chair). It is also supported by Dr. Peter Adamson (COG chair), and will leverage the largest pediatric AML tissue bank in the world, which is located at Fred Hutch in Seattle.
The initial scope of TpAML consists of two major activities with both near and long-term benefits: Build a comprehensive list of therapeutic targets via discovery-phase, large-scale, deep “omic” sequencing and analysis of 1000 pediatric patient samples. This will enable us to expand and maximize our treatment toolkit.
Profile each newly diagnosed patient’s AML, beginning the shift to personalized care, with the goal of offering clinical genomic sequencing to every young patient nationwide. Testing will also be extended to biphenotypic leukemia patients (mix of ALL & AML), a high-risk group routinely excluded from many trials. Genomic testing allows us to match all available (and emerging) therapies to a patient based on their specific cancer profile. It can also allow us to better understand why some patients respond more than others to a given therapy and will provide information for real- time, molecular level disease monitoring (more sensitive and personalized than today’s routine tests).
COG believes that both large-scale and patient-specific genomic sequencing are foundational, mission- critical activities that can uncover the drivers and vulnerabilities of pediatric AML, enabling optimized and personalized use of new therapies now and in the future. It also allows us to maximize use of existing FDA approved agents not previously considered for use in kids fighting AML.
Biomarkers to Predict Response to I-MIBG Therapy High-Risk Neuroblastoma

In January of 2017, Sammy's Superheroes Foundation funded $60,000 to the I-MIBG project by Dr. DuBois at Dana Farber Cancer Institute in Boston. I-MIBG is a form of targeted radiation that has a strong track record in treating children with relapsed neuroblastoma. Prior studies have shown that I-MIBG has one of the highest response rates in this setting. At present, approximately 50% of newly diagnosed patients with high-risk neuroblastoma will experience a relapse and ultimately die of their disease despite aggressive multi-modality therapy. In this context, moving 131I-MIBG therapy earlier in the course of therapy is a high priority to prevent relapse and death.
The Children’s Oncology Group has approved a large randomized phase III clinical trial to study the addition of I- MIBG to standard therapy for children with newly diagnosed high-risk neuroblastoma. Children who participate in this trial will either receive standard treatment or standard treatment with the addition of one cycle of I- MIBG given during the initial cycles of chemotherapy. The trial will determine definitively whether adding 131I-MIBG improves cure rates for children receiving frontline therapy.
This trial is a major undertaking and provides an unprecedented opportunity to improve the care for children with neuroblastoma. As the Children’s Oncology Group typically only conducts a study of this scale once per decade, the study team has worked hard to make sure that the neuroblastoma community will learn as much as possible during the course of the trial. Since I-MIBG therapy is complex and often requires patients to travel to a specialized MIBG center, these biomarker studies are designed to help us select those patients most likely to benefit from I-MIBG in the future. Importantly, the Children’s Oncology Group funds the conduct of the clinical trial, but the study team is responsible for raising funds to support the important biomarker tests that are embedded in the trial.
Cell Death Protein Family Profiling and Therapeutic Targeting of Regulatory T Cells
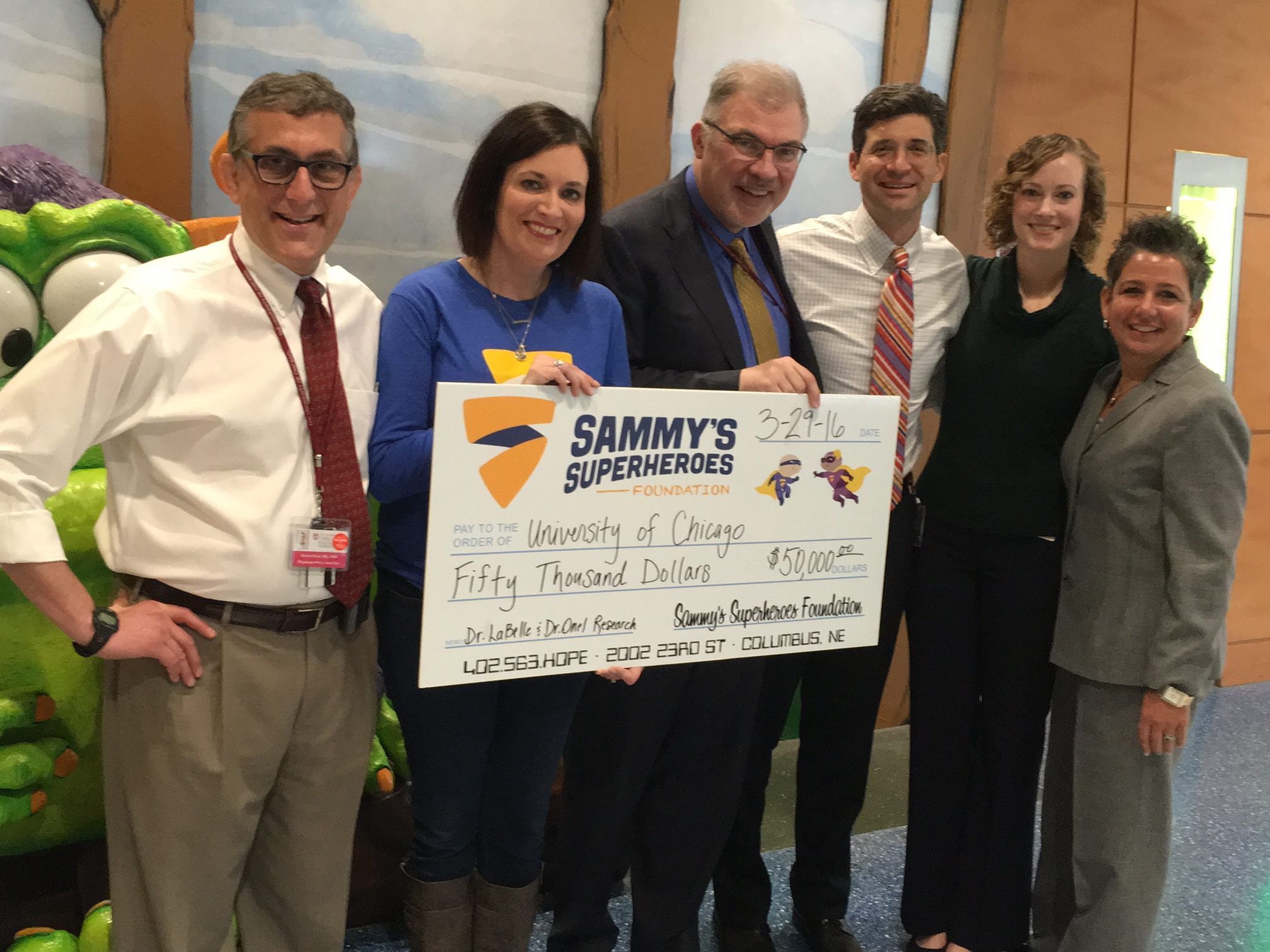
In July of 2015, we funded $50,000 towards a project titled "Cell Death Protein Family Profiling and Therapeutic Targeting of Regulatory T Cells" conducted by Dr. LaBelle at the University of Chicago. Dr. James LaBelle is working on an area of pediatric cancer research to identify innovative therapies for rare cancers through manipulating the immune system and its response to solid tumors such as Ewing’s sarcoma, rhabdomyosarcoma, neuroblastoma, and lymphoma.
A paramount obstacle in the progression of personalized forms of cancer treatment is identifying ways to promote the patient’s immune response to attack cancerous cells. To address this, Dr. LaBelle and his team are working on developing a new therapeutic strategy to stimulate immune cells to work against tumors that have gone undetected by the immune system and are otherwise refractory to conventional therapies.
In order to develop this new treatment, he is using a multidisciplinary approach spanning chemical engineering, immunology, immunotherapy, and molecular biology. The inclusion of both animal and human samples in preclinical testing greatly enhances the translational power of this approach that has the potential to affect a large number of cancer treatment strategies.
Using Novel In-Depth DNA Sequencing To Learn From Rare Tumors
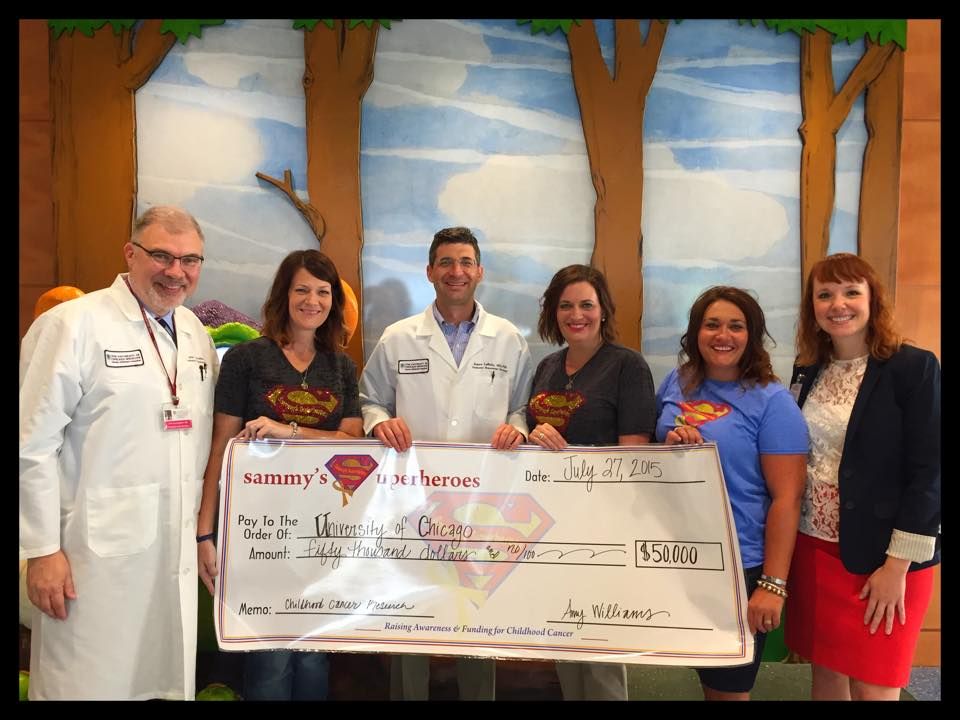
In July of 2015, we funded another $50,000 towards the project titled, "Using Novel in-depth DNA Sequencing to Learn from Rare Tumors" with Dr. Onel and Dr. Cunningham of University of Chicago.
Project Update:
"With the support of Sammy’s Superheroes and other philanthropists, Drs. Onel and Cunningham, along with colleague Navin Pinto, MD, have made significant progress. We established a formal collaboration with LIJ-NSUH-Hofstra University School of Medicine to collaborate on GREAT KIDS (Genomics of Risk Evaluation and Anticancer Treatment in Children) and to train their fellows in clinical cancer genetics. LIJ/Cohen Children’s Medical Center of New York is the 2nd largest Pediatric Hematology/Oncology program in New York, about three times the size of ours. GREAT KIDS is being submitted to the University of Chicago’s Institutional Review Board and we anticipate enrolling patients for comprehensive genomics sequencing soon. In the meantime, we are currently investigating our first two families through GREAT KIDS. Our approach to developing this platform is also the subject of a manuscript that has been selected as a Special Report in the journal Personalized Medicine. Finally, to further leverage the your investment, we just learned that we are finalists in a University of Chicago Comprehensive Cancer Center grant competition to facilitate Team Science around GREAT KIDS. In addition, The University of Chicago has partnered with Harvard, The University of Washington and The University of Texas on this project."
Improving Neurologic Outcomes in Pediatric Cancer Survivors
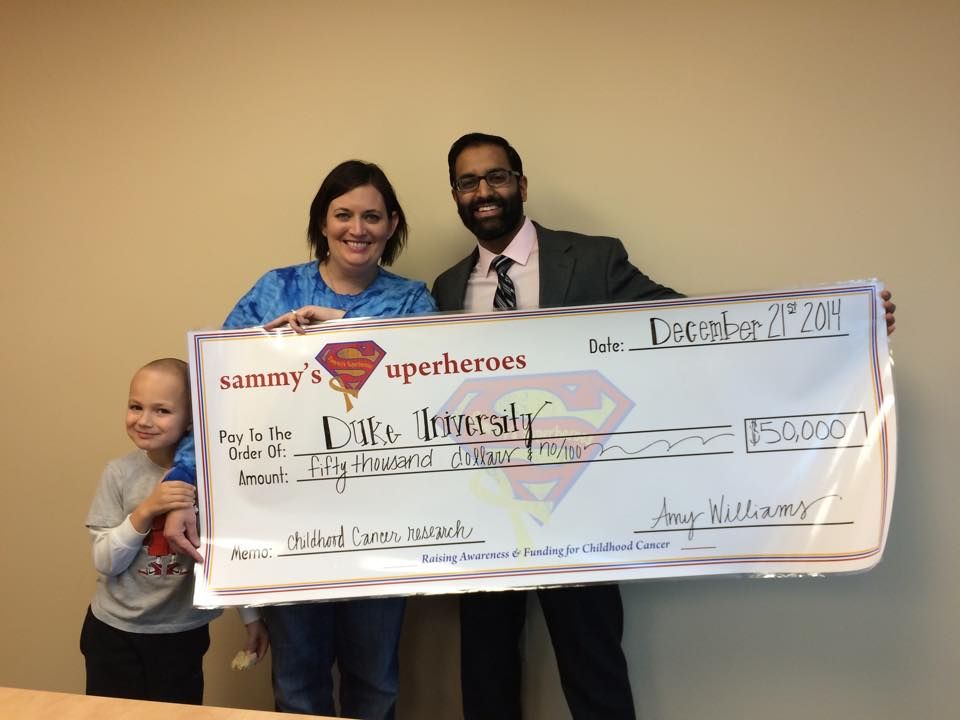
In December of 2014, our organization granted $50,000 to Dr. Sachit Patel's research project at Duke University titled "Improving Neurologic Outcomes in Pediatric Cancer Survivors."
This research is important for all children with cancer but especially children with brain tumors and other children that receive radiation to their developing brains.
The main components of cancer treatment remain a combination of surgery, chemotherapy and radiation. However, balancing maximal therapeutic benefit and acceptable toxicity remains challenging for oncologists. In particular, little can currently be done to limit acute and long-term neurologic effects related to chemotherapy and radiation.
Children are at high risk of neurologic injury related to cancer treatment due to their actively developing brains. During early childhood and adolescence, the brain undergoes dynamic changes resulting from neuronal growth, arborization, and synapse formation. Thus, pediatric cancer treatment affects the brain at the most vulnerable time in neurologic development, leading to profound adverse consequences.
This trial will begin the development of cell therapies to protect the brains of children undergoing radiation therapy as part of their cancer treatment. This research proposal builds on previous experience studying brain injury and on our successful development of human umbilical blood cell therapy products for other neurological indications. We hope this will be the foundation for future research that will ultimately allow pediatric cancer survivors to live full lives without neurologic limitations.
Whole Exam Sequencing (WES) in Neuroblastoma before and after Induction Therapy

In September of 2014, we funded $60,000 to a project titled "Whole Exam Sequencing (WES) in Neuroblastoma before and after Induction Therapy" at the University of Nebraska Medical Center conducted by Dr. Donald Coulter. WES can identify variation in the protein encoding areas of DNA. It is a method which has become more practical with lower cost and since upwards of 90% of all mutations are within the exon this allows for the identification of variation with smaller samples than with whole genome sequencing.
Currently, the extraction of cells and exosome sequencing is done. Four samples had pre chemo and post chemo data, so we are in the process of evaluating a number of genes (ones known to be involved in neuroblastoma prognosis and others that we think may play a role in chemotherapy resistance) to see if and how they were changed during chemotherapy. This is an ongoing project.
Using Novel In-depth DNA Sequencing To Learn From Rare Tumors

In January of 2014, Sammy’s Superheroes made their inaugural grant of $50,000 to the University of Chicago Medicine Comer Children’s Hospital in support of pediatric cancer research lead by John Cunningham, MD, and Kenan Onel, MD. The project is designed to better understand the molecular basis of pediatric cancers, which remain a major cause of non-traumatic childhood mortality. This deficiency occurs at least in part because of the rare nature of childhood cancer. The University of Chicago Program in Childhood and Young Adult Cancer has developed a repository of samples derived from patients with rare pediatric cancers. These cancers were chosen based on representation of the diagnostic challenges facing physicians at the bedside, the lack of response of these tumors to therapy, and their ability to reveal insights not only into childhood cancers, but also into common adult cancers. Specifically, we have focused on familial leukemias, lymphomas and sarcomas, and on rare adult cancers seen in childhood including colon, stomach, and lung carcinomas.
Under the direction of Dr. Kenan Onel, this project uses recently developed and novel DNA sequencing technologies developed at the University of Chicago to identify the genetic basis of these tumors. Our goal is to sequence 40 tumors in the first instance over a two-year period. We anticipate that the results of these studies will identify not only the DNA defects that induce the tumors, but also provide potential cell targets that will allow us to develop new therapeutic agents to treat children and adults with these devastating diseases.
